A Parent’s Guide
– To Childhood ADHD –
This is a comprehensive guide for parents to understand ADHD in children. In this guide we’ll walk you through the types of ADHD in children, symptoms of ADHD, treatment for childhood ADHD, and what parents can do to support their children.
Happy reading!

Contents
select your chapter
CHAPTER 1
What is ADHD?
ADHD stands for Attention Deficit Hyperactivity Disorder. It’s a mental health disorder affecting over 6.1 million children, according to a 2016 parent survey by the CDC.

ADHD is a neurological issue. Behaviors, including distractibility, inattention, and hyperactivity are almost involuntary and controlling them requires a lot of work and oftentimes treatment.
Estimated number of US children who ever had a diagnosis of ADHD – The Centers for Disease Control & Prevention
CHAPTER 2
Types of ADHD in Children
Although symptoms vary from child to child, there are three main types of ADHD that doctors commonly use to diagnose children.

Hyperactive or Impulsive ADHD
With this type, children show symptoms of both hyperactivity and impulsiveness, yet they are able to pay attention and aren’t easily distracted. This is the least common type of ADHD.
Inattentive or Distractible ADHD
This type usually involves inattention and distractibility without hyperactivity. Formerly known as ADD (Attention Deficit Disorder), children with this type are not overly active so symptoms may not be noticed right away.
ADHD Combined Type
This is typically the most common form of ADHD and combines both hyperactive and inattentive types.
CHAPTER 3
ADHD Symptoms in Children
Depending on the age of your child and type of ADHD they may have, ADHD symptoms can look different from child to child.
If you notice any of these symptoms lasting longer than 6 months and in several areas of your child’s day to day life, seek help from your primary care physician or a mental health specialist.

Signs of ADHD in Babies (Ages 0-1)
In most instances, ADHD isn’t diagnosed in children until they reach the age of 4. It’s normal for all babies to kick, cry, play, and exhibit other signs of fussiness. This doesn’t necessarily mean, however, they have ADHD.

Signs of ADHD in Toddlers (Ages 1-3)
Physical Signs
- Fidgets or squirms often
- Restlessness or need for continual movement
- Interrupts or intrudes on others
- Aggressive behavior while playing
Behavioral Signs
- Problems with sustained mental engagement
- Easily distracted
- Difficulty following through
- Loses things often
- Forgetful in daily activities

Emotional Signs
- Impatience with others
- Extreme emotional outbursts (including anger, frustration, anxiety, and overwhelm)
- Easily frustrated and/or irritable
Signs of ADHD in Children (Ages 4-8)

Physical
- Fidgeting or squirming while sitting
- Excessive talking
- Interrupts others while talking or playing
Behavioral
- Has trouble waiting their turn
- Difficulty focusing in class
- Difficulty paying attention during conversations or discussions
Emotional
- Worries excessively over small things
- Trouble calming down when angry or annoyed
- Easily frustrated
Signs of ADHD in Pre-Teens (Ages 9-12)
Physical
- Hyperactivity and fidgeting
- Changes in appetite
- Talking excessively
Behavioral
- Lack of focus or easily distracted
- Aggressive behavior
- Impulsive or poor decision making
- Self-harm (such as cutting)

Emotional
- Difficulty regulating emotions
- Feelings of worthlessness or guilt
- Anxiety
*all symptoms may be aggravated during puberty
Signs of ADHD in Teenagers (Ages 13-19)

Physical Signs
- Increased impulsivity (while learning to drive, engaging in sexual activity, or forming new relationships)
- Substance Use & Abuse
- Sleep Problems (sleeping too much or not enough)
Behavioral Signs
- Learning Problems
- Inattentive or Excessively Attentive
- Consistent Refusal to Listen to Adults or Authority Figures
Emotional Signs
- Anxiety
- Depression
- Loss of interest in usual activities
CHAPTER 4
Causes of ADHD in Children
While there is no known cause of ADHD, factors including genetics and environmental exposure during the developmental stage are known to play a key part in children with ADHD.
Genetics
ADHD commonly runs in the family.
A blood relative such as a parent or sibling with ADHD or other mental health disorder may increase the likelihood of your child developing ADHD.
Environmental
Toxins in the environment are a contributing factor for ADHD in children.
Lead paint in an old house, as well as chemicals in food, carpeting, and other household products can increase the risk of developing not just ADHD but autism and learning disabilities.
Situational
Premature birth or exposure to alcohol, drugs, or nicotine during the prenatal phase is also a risk factor in ADHD in children.
CHAPTER 5
When to See a Doctor for Childhood ADHD
ADHD in children can be diagnosed as early as age 4. And though there is no single test to diagnose ADHD in your child, if symptoms persist for more than 6 months, it may be time to see a doctor.
Be prepared with additional information from your child’s teachers or other caregivers when seeking help as this will give the doctor a clearer picture of your child’s pattern of behavior.
Who Can Diagnose Childhood ADHD?
Primary Care Physicians
- Pediatricians
- Nurse Practitioners
- Physicians Assistant
Mental Health
- Child Psychologist
- Child Psychiatrist
- Licensed Counselor
- Marriage & Family Therapist
Specialists
- Neurologist
- Occupational Therapist
- Behavioral Therapist
- Speech & Language Therapist
CHAPTER 6
How Is ADHD Diagnosed in Children?
A lot of people like to self-diagnose their children with ADHD, but one has to be diagnosed by a healthcare professional. So how is a child diagnosed with ADHD?

According to the CDC, primary care and mental health providers diagnose ADHD using the guidelines set by The American Academy of Pediatrics.
Because there is no single test for ADHD, healthcare professionals use medical exams and standardized rating scales by gathering information from several sources, including parents, teachers, and other family members.
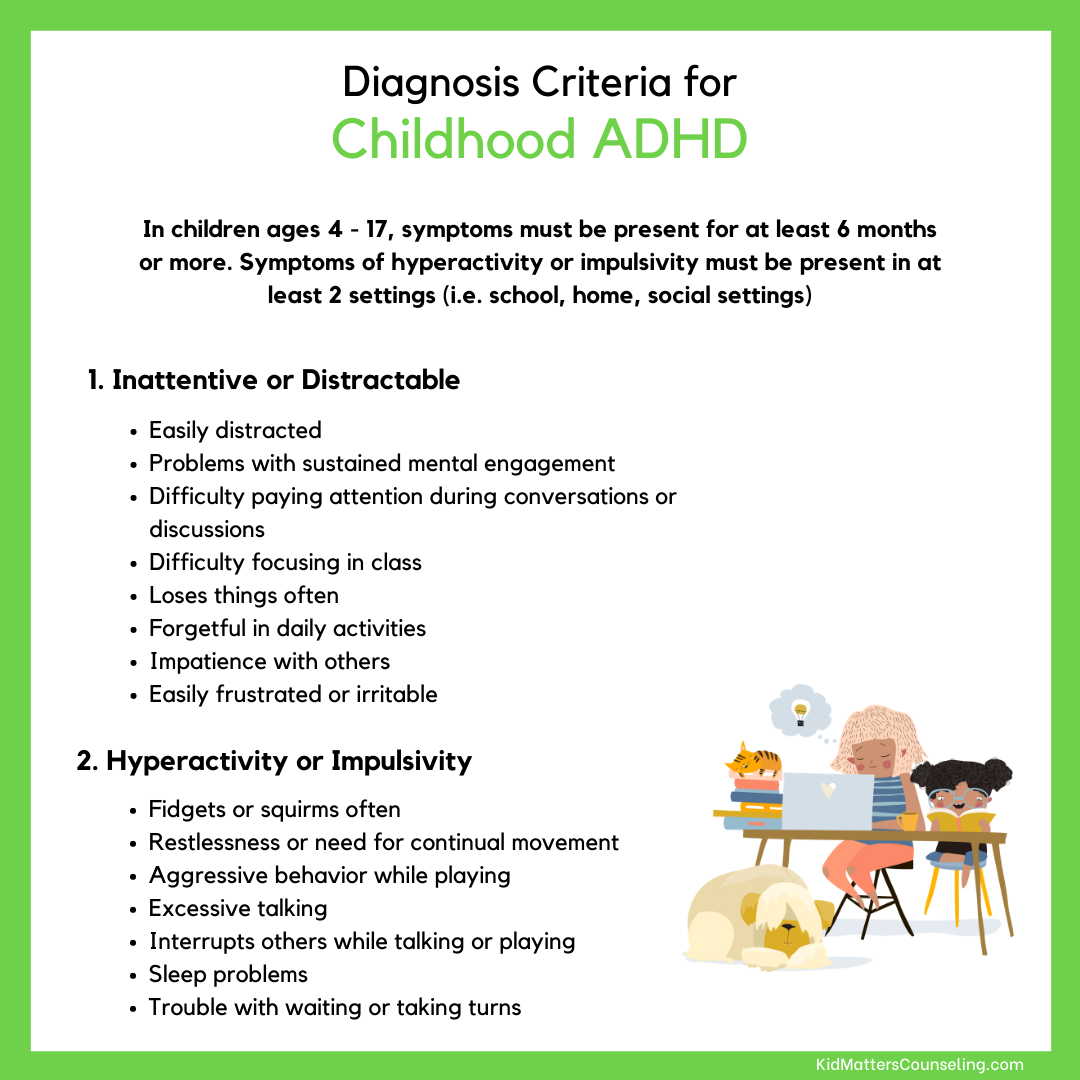
Diagnosis Guidelines:
- Symptoms of hyperactivity or inattention that last longer than 6 months
- Symptoms of hyperactivity or impulsivity that is present in at least 2 settings (i.e. school, home, social settings, extracurricular activities)
- Symptoms interfere with your child’s daily activities and relationships
- In children ages 4-16, six or more symptoms must be identified (see Chapter 3)
- In children 17 or older, five or more symptoms must be identified (see Chapter 3)
Exams Can Include:
- A medical history of both the child and other family members
- Aptitude and intelligence evaluations
A complete physical exam, including vision, hearing, and motor skills - A brain wave scan called the Neuropsychiatric EEG-Based Assessment Aid (NEBA) System
No matter when (or how) your child is diagnosed with ADHD, there’s a wealth of treatment options to choose from. In the next chapter, we discuss several ways to help alleviate your child’s ADHD symptoms both with medication and without.
CHAPTER 7
Treatment for ADHD in Children
without Medication
Disclaimer: In this section, we discuss homeopathic medication, as well as nutritional and supplemental advice.
Please consult your primary care physician before adding or removing foods, vitamins, essential oils, or supplements to your child’s healthcare routine.
Behavioral Therapy for ADHD

Behavioral Therapy for ADHD in children helps them manage their inattentiveness and hyperactivity, as well as their self control and self-esteem issues.
The skills taught in behavioral therapy can be used with or without medication and are most successful when practiced consistently outside of therapy sessions with a parent or caregiver.
**For more information on how therapy can help Childhood ADHD, check out this episode of the Parent Matters Podcast with guest Dr. Lauren Smith.
Therapy Approaches That Include the Teaching of Emotional Regulation
When children experience strong emotions it’s often difficult for them to calm down. In children with ADHD, regulating their emotions is even more of a struggle leading to frequent tantrums and meltdowns.
Although meltdowns are difficult for parents, it is important to consider how the child feels. They likely feel overwhelmed and out of control!
Therapy approaches that include emotional regulation can help your child name their emotions, which in turn helps them feel more in control when big emotions pop up.
Need more? For a fun and interactive way to keep your children regulated and help them tackle their big emotions, download our FREE ebook, Teapot Regulation.
Occupational Therapy for ADHD

Occupational therapy for children with ADHD helps them improve their self-care skills, gain strength for active play, and improve the skills needed to succeed in school.
An Occupational Therapist will also work closely with parents and caregivers to arm them with the tools to confidently manage their child’s unique needs.
Nutrition for Children with ADHD
In children with ADHD, their diet may be contributing to their symptoms. Diets high in sugar and carbohydrates cause their blood sugar to spike, leading to increased bouts of hyperactivity. To combat this, include high protein meals in their daily diet.
Some foods to try:
- Peanut butter (or another nut/seed butter if allergic)
- Eggs
- Tofu or soy
- Lean poultry or fish
- Lean meats
- Beans & Legumes
Foods to avoid:
- High calorie snacks like chips
- High sugar foods such as cookies, cakes, and sodas
- Chemically processed foods with additives, preservatives, and dyes.
- High sensitivity foods like dairy, nuts, and wheat

Natural & Homeopathic Medicine
for Childhood ADHD
Supplements
There are many alternatives to medication when treating your child for ADHD. If you want to take a more natural approach to managing your child’s ADHD symptoms, supplements may be the way to go.
Supplements can include:
- Vitamins – multivitamins, fish oil, vitamin C or D, and melatonin
- Minerals – zinc, magnesium, and iron
- Herbs – lemon balm, ginkgo biloba, and St. John’s Wort


Essential Oils
Essential oils are concentrated plant extracts and are used to improve both mental and physical health. When using essential oils for children, make sure to lower the recommended dose and dilute with a carrier oil such as coconut or olive oil when applying to the skin.
**Avoid giving essential oils sublingually (under the tongue) or orally.
Essential oils for ADHD include:
- Lavender – for relaxation and decreased anxiety
- Ylang Ylang – for calming
- Frankincense – for an immune system boost
- Peppermint – for mental focus
Exercise & Mindfulness Practices
for Childhood ADHD
Exercise, meditation, and mindfulness techniques have been proven to improve mental health in adults and children alike.
If your child has been diagnosed with ADHD, using some of the strategies below may help you find creative ways to redirect your child’s focus.
Exercise
Physical activities such as gymnastics, basketball, martial arts, and even yoga help your child burn excess energy. When children with ADHD participate in sports, they learn to not only use their body, but to focus their mind, manage their hyperactivity, and gain a sense of self-confidence.
Some other activities to try:
- Swimming
- Biking
- Dance
- Strength Training (lifting weights, jump rope, pushups, etc.)

Meditation & Mindfulness
We all know that meditation and mindfulness are great techniques for adults to lower stress and anxiety, but did you know that it works for children as well?
Mindfulness in children with ADHD has been shown to have similar results as daily medication. It increases focus and attention while reducing stress and anxiety.
One therapeutic approach that parents may find helpful is Acceptance and Commitment Therapy. ACT is a therapeutic approach heavily based in mindfulness.
It involves learning and working towards being able to accept who you are and begin to shift to a more compassionate stance when dealing with ADHD symptoms.
**For tips on how to practice mindfulness with your kids, check out the FREE Guide, 25 Ways to Practice Mindfulness
Screen Time
Children with ADHD can spend hours on their screens or playing video games without realizing it. Excess screen time affects your child’s sleep patterns, which contributes to exacerbating their ADHD symptoms.
It affects their social development and if we’re not careful, their safety.
When children are given free reign on their devices, this can lead to inappropriate imagery and content not suitable for their age. It’s important to set clear rules and expectations when it comes to screen time for your child.
One way you can do that is by using a Screen Time Contract.
At Home Techniques for Parents
Parenting an ADHD child is exhausting. Your day is filled with looking for things your child ‘lost’, dealing with careless mistakes, selective listening, fidgeting, and epic amounts of redirecting distractibility. And that list is only a small selection of all that you really have to deal with.
There are always many other symptoms experienced due to multiple factors; the possibility of multiple diagnosis, your child’s biology, personality, environmental settings and life transitions. It’s child management taken to a whole new level as a parent or caregiver.

You long to see your child succeed but the time you spend redirecting and coaching towards that success seems endless.
Here are four techniques to implement in your everyday life to help manage the unpredictability of ADHD.
Create Routine
All children thrive on routine, but especially those with ADHD. Creating a consistent routine helps them anticipate their day, gives them a sense of control, and can reduce daily distractions.
It might be helpful to get out post-it notes or a wall calendar and, with your kiddos, write down all the new routines that will happen for the week. Then plan out how these new routines will take place.
Communicate
Keep the lines of communication open with your child. Children with ADHD often interrupt or speak out of turn.
Educate them on feeling words and then label together feelings that come or may come when they’re feeling angry, stressed, or overwhelmed.
Talk about where it starts in the body and ways those feelings can present themselves.
Follow Through
If your child is seeking help from a doctor or mental health professional for their ADHD, it’s important to continue to use the techniques provided by your therapist even when the sessions have ended.
Managing ADHD is a team effort and all players are working towards creating space for your child to be confident and happy.
Have Fun
Managing ADHD is stressful for both you and your child and it’s important to set aside time everyday to have fun.
Get down to their level and finger paint or go for a bike ride. Maybe read together or bake a healthy snack.
Creating that special time together increases their self-confidence and self-esteem and further strengthens your parent-child relationship.
For more ideas on how to connect with your kids, click here to sign up for our FREE 5-day Parenting Challenge!
CHAPTER 8
Common Medications for
Childhood ADHD
Disclaimer: In this section, we discuss the most commonly used medications to treat ADHD in children.
This is just a small sampling of available treatment options.
Please consult your primary care physician for the right medication to treat your child’s ADHD symptoms.

When researching medications for treating your child’s ADHD symptoms, you may be overwhelmed with the amount of information you find. Stimulant vs. non-stimulant, methylphenidate vs. amphetamine, and even immediate release vs. extended release. It can be confusing to know which route to go.
Immediate Release Medication vs. Extended
Release Medication
Immediate release (or short-acting) medications usually take effect within 30-45 minutes and doses are taken every 3 to 4 hours, with some of the newer medications lasting up to 8 hours.
Extended release (or long-acting) medications are typically a once-a-day pill taken first thing in the morning and symptom relief should last all day.
Methylphenidate vs. Amphetamine
Both methylphenidate and amphetamine are central nervous system stimulants used to treat the impulse control associated with ADHD in children. There’s no evidence that one is better than the other, however, it’s been said that amphetamines tend to be stronger and last longer than methylphenidate.
Common Methylphenidate Medications for Childhood ADHD:
- Ritalin (short-acting)
- Focalin (short-acting)
- Metadate (long-acting)
- Concerta (long-acting)
- Quillivant (long-acting)
Common Amphetamine Medications for Childhood ADHD:
- Adderall (short-acting)
- Dexedrine (short-acting)
- Adderall-XR (long-acting)
- Dexedrine Spansule (long-acting)
- Vyvanse (long-acting)


Benefits of Stimulant Medications for ADHD in Children Can Include:
- Improved focus
- Improved impulse control
- Reduction in hyperactivity
Side Effects of Stimulant Medications for ADHD in Children Can Include:
- Trouble sleeping
- Decrease in appetite
- Headaches
- Changes in mood
- Developing tics (eye blinking, head movements)
- Stunted growth
- Visual hallucinations
Stimulant vs. Non-Stimulant Medication for Childhood ADHD
Stimulant medications like the ones listed above (Ritalin, Focalin, Adderall, etc.) are some of the top choices in treating childhood ADHD. However, if your child is not responding well, is experiencing an increase in side effects, or has a pre-existing medical condition that prohibits the use of stimulants, then non-stimulant medications are an alternative.
In most cases, these medications are used to treat conditions such as depression or high blood pressure, but doctors have found that they also help alleviate symptoms of ADHD. Regular checkups are crucial when taking non-stimulants to monitor your child’s blood pressure, heart rate, and liver functionality.
Common Non-Stimulant Medications for Childhood ADHD:
- Strattera
- Wellbutrin
- Catapres
- Tenex
Side Effects of Non-Stimulant Medications for Childhood ADHD:
- Decreased Effectiveness (can take up to 6 weeks to take effect)
- Dizziness
- Headaches
- Vomiting
- Nausea
- Tiredness
- Heart/Liver Issues

CHAPTER 9
4 Most Common Myths About
Childhood ADHD
With the internet at our fingertips, it’s easy to get our questions answered with the click of a button. But that can also lead to misinformation, confusion, and information overload.
Here we tackle four of the most common myths surrounding childhood ADHD.

Myth: ADHD Can Be Cured
Attention Deficit Hyperactivity Disorder is a chronic mental health condition. According to the Centers for Disease Control and Prevention, “ADHD is one of the most common neurodevelopmental disorders of childhood. It is usually first diagnosed in childhood and often lasts into adulthood.”
While there is no cure for ADHD, symptoms can be managed using one or a combination of the information discussed on this page.
Myth: ADHD Is Caused By Bad Parenting
Although some people think that social factors or poor parenting may cause ADHD, research studies point to genetic and neurological factors as the main causes of ADHD.
In fact, twin studies have shown that family environments contribute very little to individual differences in ADHD symptoms. Family environments and parenting patterns do, however, largely impact coexisting disorders such as oppositional defiant disorder or other ADHD symptoms.
Although there are many changes parents can make to support their child with ADHD, their parenting did not cause the diagnosis nor can they reverse it.
Myth: My Child is Choosing Not to Pay
Attention to Me
Parenting a child with ADHD is hard and can be frustrating. Morning routines are stressful, chores may feel impossible, and don’t forget about homework time.
Oftentimes, parents and teachers assume that the child is deliberately choosing to disobey or not follow through with instructions. But that is usually not the case.
ADHD is a neurological issue. Their behaviors, distractibility, inattention, hyperactivity are almost involuntary and controlling them requires a lot of work and oftentimes treatment.
Many kids who may get started on a task, then get distracted by something (anything), which gets them off course. They may then need to be directed (and re-directed) repeatedly until the task is complete. They do not choose to get distracted, to forget, to lose things, to have trouble finishing tasks, so it’s important for parents to understand and have empathy for their distractible child.
Myth: My Child is Just Lazy
Many families believe that their child doesn’t have ADHD because they’re not hyper or constantly moving.
In actuality, if your child has the Inattentive (or Distractable) form of ADHD, they won’t display any symptoms of hyperactivity. This type is defined by difficulty sustaining attention and being easily distracted.
Oftentimes, it gets overlooked because symptoms aren’t recognized right away. It’s easier to notice the child who is constantly moving and overactive rather than the child who is quietly daydreaming.
However, overlooking inattentive kids with diagnosable ADHD can have serious and lasting consequences.
CHAPTER 10
Parenting Support for
Childhood ADHD
When parenting a child with ADHD, your day consists of managing schedules and routines, as well as staying up to date on medications and doctor appointments. This can leave little time for making sure your own needs are met.

It can lead to:
- Increased individual and marital stress
- Anxiety
- Depression
- Feelings of powerlessness
The best way for you to take care of your child is to also take care of yourself.
Some ways to lower stress:
- Do something just for you everyday
- Set achievable daily goals for yourself
- Take a break when you need it
- Practice meditation/mindfulness
- Keep a daily gratitude journal
- Delegate tasks to other family members
Resources
Try as we might, we can’t always do it alone. Seeking help from your community, doctors, and online resources can arm you with the tools to help manage your daily struggles as a parent to a child with ADHD and assist in lowering your stress, anxiety, and depression.
Here are some resources to try:
Parent support groups
Seek advice from a mental health professional
-
- Individual counseling
- Couples counseling
Phone a friend
-
- Do you know another parent who’s going through a similar situation? Give them a call and offer each other support as you navigate the trials of ADHD.
Final Thoughts

Parenting a child with ADHD can be a struggle. We hope that by providing you with the strategies, techniques, and resources discussed on this page, it makes your job a little bit easier.
If you feel you could use some additional support creating a custom treatment plan for your child, click below to schedule an appointment with one of our child therapists today!
Kid Matter Articles on ADHD
Holiday Gift Giving Ideas for Kids Under $20
The holiday season is fast approaching, and finding the perfect gifts for kids can be a challenge. But fear not! We've got you covered with our 2023 Holiday Gift Ideas for Kids Under $20. We've curated a list that is sure to bring joy and excitement to children...
3 Fun Relaxation Activities for High-Energy Kids
For many young children, most mindfulness activities can require too much stillness for a child who is on the go. Calming your body, however, doesn’t have to be stagnant. When kids’ bodies feel out of control, they need help to become more grounded. When a child...
How to Know When Your Child Needs a Neuropsychological Evaluation for ADHD
In this week’s episode of the Parent Matters Podcast, Susan is joined by Dr. Sandy Kruse, Licensed Clinical Psychologist and Director of the Heritage Diagnostic and Assessment Center. They talk about how to know when your child needs a neuropsychological evaluation...
New Clients Call: (855) 586-1802
Current Clients: (855) 543-7687
Ask Us Anything!
We help anxious kids and frustrated parents. We serve Hinsdale & the Western Suburbs of Chicago.
Made with ♥︎ in Hinsdale, Illinois for Chicago
Built By Brand Your Practice.
Kid Matters Counseling, P.C. DISCLAIMER: This website and blog are for informational, educational and general discussion purposes only. It is understood that no guarantee or warranty arises from the information provided, discussed or commented upon in this website and blog nor does it constitute legal or other professional advice on any subject matter. Access to this website and blog is voluntary and at the sole risk of the user. If you think that you have a medical emergency (including clinical), call your doctor or 911 immediately. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. While the information contained within this website and blog is periodically updated, no guarantee is given that the information provided is correct, complete, and/or up-to-date. See our complete Privacy Policy and Terms of Service.